Endometrial cancer is one of the most common cancers of the uterus that originates in the lining of the uterus, also called the endometrium. It is one of the most common forms among females, primarily beginning after menopause. Generally speaking, uterine cancer includes malignancies that develop within the uterus and encompass a wide range of illnesses, from endometrial cancer to uterine sarcoma, a rare tumour of the muscular wall of the uterus. About 95% of uterine cancers, however, are endometrial; hence, it is usually the form discussed. Understanding Uterine Cancer Types
Endometrial Cancer: This is the most common form of gynecologic cancer, and it includes the lining of the uterus. It accounts for the majority of cancers of the uterus. If found early, the outcomes of endometrial cancer are usually good; however, risk factors and symptoms can be quite variable, and awareness is critical.
Uterine Sarcoma: Uterine sarcoma is a very uncommon type of cancer that originates in the myometrium, the uterine muscle layer. These cancers often require different treatments and are usually more aggressive and more likely to spread.
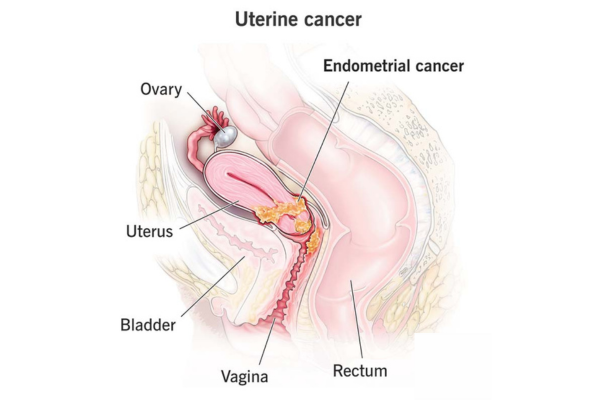
Function and Structure of the Uterus
The uterus is the major portion of the female and AFAB reproductive system, and it is where the fetus develops during pregnancy. It is divided into two main parts:
The upper part, the corpus, constitutes the major portion of the uterus. The lower portion, the cervix, connects the uterus to the vagina. Cancer of the uterus typically begins in the corpus; cancer of the cervix, though related, is a different form of cancer and affects only the cervix.
Endometrium: What It Does and How It Changes with Time?
The endometrium is a tissue layer that lines the inner wall of the uterus and changes throughout the cycle of hormonal changes. Estrogen and progesterone thicken the lining of the endometrium in preparation for a possible pregnancy. During a cycle when pregnancy does not occur, the level of progesterone decreases and the lining of the endometrium is sloughed off, resulting in menstruation.
Prevalence and Risk
Endometrial cancer is the most common reproductive cancer in women and AFAB individuals. Risk increases after menopause and it is estimated to affect 3% of women. It is currently estimated that 65,000 people are diagnosed with endometrial cancer every year.
Signs, Symptoms, and Early Warning Signs
Uterine cancers can have similar symptoms as other gynecologic cancers so paying attention to early signs is important:
- Pre-menopausal bleeding: Bleeding between periods can provide a clue to some uterine abnormalities.
- Post-menopausal bleeding: Any spotting after menopause is already a warning sign.
- Continuing abdominal pain: Unexplained cramping especially in the lower abdomen can hint at uterine cancer.
- Unusual discharge: Sometimes there is clear or white discharge after menopause.
- Heavier-than-usual bleeding the woman is above 40: Prolonged frequent bleeding can also be a warning sign.
- Early detection and professional diagnosis make the treatment much more effective.
Understanding the Causes of Uterine Cancer
Though specific causes are yet to be known by researchers, uterine cancer results from mutations in uterine cells, causing them to proliferate abnormally and develop into tumours. However, several risk factors increase the possibility of uterine cancer due to hormonal influences, genetic factors, or other lifestyle factors.
Key Risk Factors
Hormone-Related Risks The risk associated with endometrial cancer may be determined by the balance of hormones, especially estrogen and progesterone. Several conditions and treatments might affect the levels of these hormones. These include:
- Obesity: The excess amount of body fat alters the levels of production of these hormones, raising the levels of estrogen.
- Polycystic Ovary Syndrome (PCOS): This condition disrupts the balance of the body's hormones. It can raise the risk of this cancer.
- Estrogen Therapy without Progesterone: The use of unopposed estrogen raises risks since it prolongs the exposure.
Genetic Factors
- Lynch Syndrome: This genetic disorder, passed along in families, increases the risk of endometrial and some other types of cancer.
Lifestyle and Age
- Age: Uterine cancer mostly occurs in people above the age of 50.
- High-fat diet: Diets high in animal fat are associated with an increased risk of cancer, and this can lead to obesity, which is an independent risk factor.
Other Health Conditions
- Diabetes: There are reports indicating diabetes independently carries a small risk of uterine cancer independent of the body mass index.
- Ovarian Tumors: Some ovarian tumours raise the levels of the hormones estrogen and progesterone, which further elevates risk.
Reproductive History
Early Menstruation before age 12 and late menopause post-50 extend the length of time a woman is exposed to estrogen.
Never being pregnant raises risk since pregnancy briefly lowers a woman's exposure to estrogen.
Previous Treatments
- Pelvic Radiation Therapy: Prior radiation exposure to the pelvic area can affect the DNA of uterine cells.
- Estrogen Replacement Therapy (ERT): Women who currently receive ERT without progesterone are at increased risk.
- Tamoxifen Use: This is a medication used in the treatment of certain cancers; it stimulates the uterus just like estrogen would.
Possible Complications of Endometrial Cancer
The prognosis of endometrial cancer is usually good provided it is treated early. The complications, however, can be serious and include:
- Anaemia: This could result from excessive bleeding.
- Cancer Spread: If left uncared for, cancer may spread to other parts of the body.
- Resistant Treatment: The cancerous cells may sometimes become resistant to treatment, requiring a different mode of treatment.
Diagnosis of Uterine Cancer: Procedures and Tests
If the symptoms persist then, being on time with the doctor is crucial.
Diagnosis can be performed by the following process:
Symptom history and physical examination: These help doctors determine the history of symptoms and risk factors.
Pelvic examination: It is a way to check the abnormality of the pelvic area.
Testing for Diagnosis
Diagnosis can be done using one or more of the following tests:
Blood Tests
- CA-125 Assay: CA-125 protein level detection because higher levels may be associated with cancer.
Imaging Tests
- CT scans: Detectors and computers use X-rays to provide detailed pictures of the inside of the body for tumour detection.
- MRI: It involves the use of magnets and radio waves to obtain internal images.
- Transvaginal Ultrasound: It provides pictures of the uterus through a special probe.
Tissue sampling procedures include:
Endometrial Biopsy: A little tissue is taken from the endometrium.
Hysteroscopy: A scope is inserted to view and take pictures inside the uterus.
D&C: Surgical removal of tissue from the uterus, to be examined.
Where cancer cells are present after tissue sampling, a pathologist classifies the type of cancer and its degree of aggressiveness to help decide on the appropriate treatment.
Type and Stage of Endometrial Cancer
Endometrial cancer is typed by kinds and stages as described below:
- Type 1: This is generally less aggressive and less apt to spread.
- Type 2: This type of cancer is usually more aggressive and often needs extensive treatment.
Stages of Cancer Uterine cancers are staged from Stage I, confined to the uterus, to Stage IV, where the cancer has spread to distant organs. Staging will help in the formulation of an appropriate treatment plan.
Treatment Options
The treatment for endometrial cancer will depend on the type of cancer, the stage of the disease, and the general state of health of the patient.
Treatment modalities include:
Surgery: This usually takes the form of a hysterectomy, which involves the removal of the uterus through:
Abdominal or vaginal route: The route used depends on the accessibility of the uterus and the extent of the cancer spread.
These can include laparoscopic surgery or robotic surgeries. In the case of Bilateral Salpingo-Oophorectomy, the ovaries and fallopian tubes are removed to prevent the spread of cancer.
- Lymph Node Dissection: This generally identifies whether the cancer has spread into the lymph nodes. Other treatments, many used in combination, include:
- Chemotherapy: This treatment utilizes drugs to kill the cancerous cells.
- Radiation Therapy: The use of beams of radiation focused on the cancerous cells.
- Hormone Therapy: The treatment consists of the balance or blockage of hormones that slow down the growth and spread of the cancer.
- Immunotherapy: This enhances the body's immune system to fight cancer cells.
- Targeted Therapy: Administers small molecules of pharmaceuticals to stop the growth of cancerous cells.
Surgical Side Effects and Recovery
Potential post-surgical side effects include the inability to conceive the induction of menopause if ovaries are removed, and related symptoms such as nocturnal sweats or dryness.
Uterine Cancer Prevention
It may not be able to be completely prevented, but you can lower your risk by exercising to keep weight down and controlling diabetes.
You can take hormonal contraceptives that contain the hormone progesterone, which adds extra protection.
Discussion of ERT options with a provider, given the use of estrogen alone, may increase risks.
Screening and Monitoring
At this time, there is no specific screening for uterine cancer. Those individuals who are considered to fall into the high-risk category may be tested periodically or receive biopsies annually after age 35 to monitor for early changes.
Prognosis and Survival Rates
The five-year survival rate in relation to endometrial cancer is approximately 81%, increasing to 95% if the condition is found early. If the cancer has already spread outside the uterus, the five-year survival rate decreases to 17%. The key is being observant and seeking health providers early for the most positive outcomes of the disease.
Frequently Asked Questions (FAQ)
What is believed to be the primary cause of uterine cancer?
Uterine cancer can be triggered by various causes, including hormonal influences or genetic conditions.
How does uterine cancer differ from cervical cancer?
Uterine cancer primarily involves the corpus; cervical cancer involves the cervix. Each demands different screenings and treatments.
How can I reduce my risk?
Maintain a healthy weight, manage diabetes and other medical conditions, and use hormone therapy only as prescribed. This may assist in lowering risk.
How does uterine cancer spread?
If left untreated, it may spread to the tissues of nearby organs or distant organs like the lungs and liver.
Final Words
Early detection remains key in the treatment of endometrial cancer. While all those with symptoms should seek a doctor, those with greater risk factors may wish to consider monitoring and risk-reducing strategies.
